eHealth: slow rate of development meets growing interest
EPR as an opportunity for improved networking
InfoSocietyDays
Team: Lukas Golder Cloé Jans Daniel Bohn
The eHealth Barometer survey has been complied and prepared as part of InfoSocietyDays since 2009. It incorporates the answers of both health care professionals and the resident population and investigates the current status and developments in the area of eHealth in Switzerland.
With the adoption of the Federal Act on the Electronic Patient Record (EPR) in June 2015, Switzerland’s parliament has now set a milestone in the implementation of eHealth in the country. The Federal Act on the EPR has been in force since April 2017, with hospitals being the first required to implement the EPR from 2020. Nursing homes and birthing centres are obligated to introduce the EPR from April 2022. The (core) associations, the future providers of the EPR, are currently at the development stage. The federal government and cantons anticipate that the EPR will be available in all regions of Switzerland from spring 2020. The introduction of the EPR is complex and requires cooperation between numerous players in the health care sector.
In many respects, the EPR represents the spearhead of eHealth efforts in Switzerland. The topic is therefore a special focus area of the monitoring activities. The study is based on the “eHealth Switzerland strategy” and the basic investigations of the European Commissions on the monitoring of eHealth. The Swiss eHealth Barometer is supported by the following partners:
Main partners: Federal Office of Public Health (FOPH), Swiss Medical Association
Co-study partners: CURAVIVA Switzerland, pharmaSuisse, eHealth Suisse, Spitex Switzerland, Careum Foundation, Ärztekasse, Department of Health of the Canton of Zurich, Department of Health of the Canton of St. Gallen, eHealth Interest Group.
Details of the sample and methodology can be found in the information below at the end of the cockpit.
Digitisation in general:

Digitisation is advancing in many areas of life and changing them irrevocably. The health care sector is also being affected by this change, but the changeover from analogue to digital solutions is in some cases taking place somewhat more slowly than in other spheres of life. This is in part because health care is a sensitive area that is at least partially regulated by authorities.
Like the resident population, it increasingly tends to be the view held by hospitals, in particular, that the Internet represents quite an opportunity or a great opportunity with respect to usage in connection with health information. Since last year, positive assessments from hospitals have even increased by around a further 10 percentage points.
The assessment of all other health care professionals was also predominantly positive here. Their assessment increased once more for the first time since 2016 and thus stands at a similar level to that recorded in 2014 when the initial measurements were taken. The least convinced health care professionals were doctors with their own medical practice. With just under 50 percent viewing the use of the Internet for health information as an opportunity for citizens, slightly less than the majority were positive in their view.

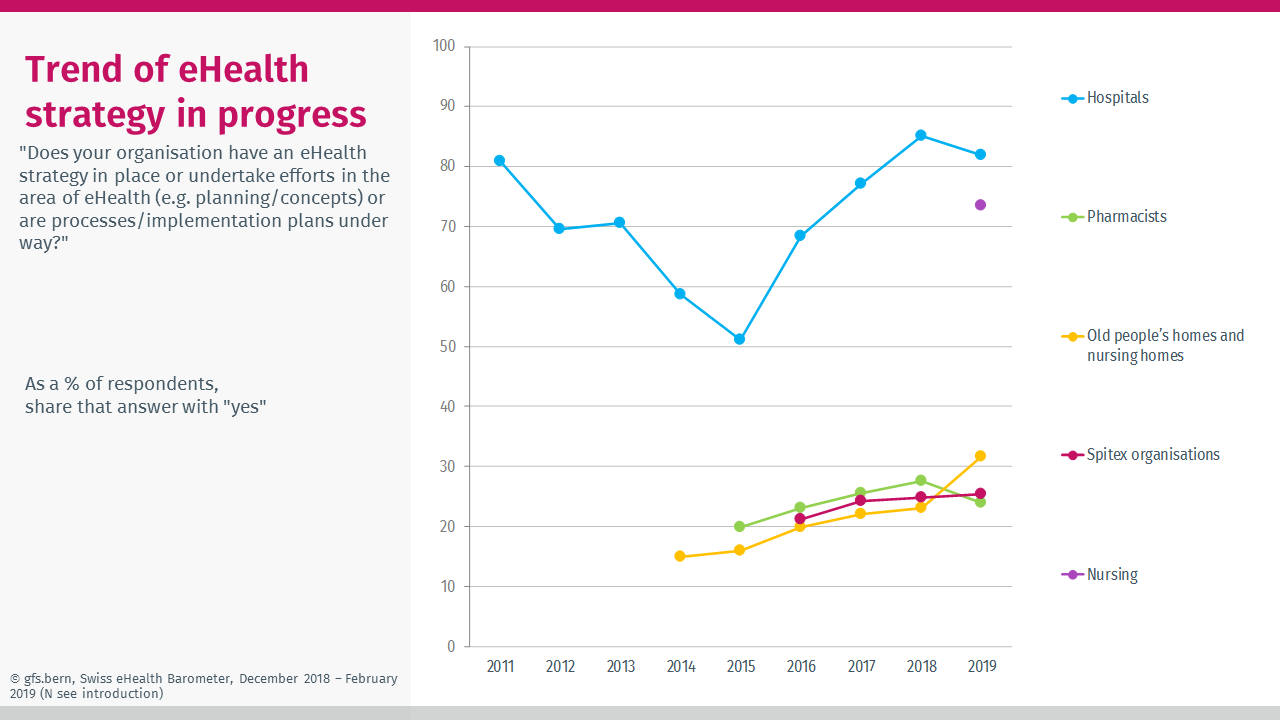
2015 represented a milestone for eHealth in Switzerland, a fact that is particularly apparent among the country’s hospitals. It appears that these institutions took the opportunity presented by the future introduction of the EPR to take a holistic view at the topic of eHealth. This becomes particularly apparent when looking at the response as to whether their organisations had an eHealth strategy, with more than 80 percent of those responsible for eHealth at hospitals answering in the affirmative. This is primarily because hospitals and nursing homes are the first groups of health care professionals to be required to offer the EPR from 2020 and 2022, respectively. In 2019, however, this value is slightly lower than was the case in 2018.
Nursing managers at hospitals, who were surveyed for the first time and likewise work in a hospital environment, also reported a particularly high proportion of eHealth strategies at their organisations at more than 70 percent. While the remaining health care professionals are still a little less advanced with respect to their eHealth strategies and efforts (old people’s homes and nursing homes: 31 percent, Spitex: 25 percent, pharmacists: 24 percent), the results recorded for these groups have been increasing slowly since the start of the survey.
Electronic documentation:
As in previous years, electronic documentation is becoming ever more established and is gradually replacing analogue methods used for the documentation of health data. At the top of the list with respect to the use of an electronic system for the saving of patient data are hospitals (96 percent) and pharmacists (86 percent). These are following by hospital doctors and nursing managers, who are likewise active in a hospital environment.
The greatest increase has been recorded for non-profit Spitex grassroots organisations, which have an electronic documentation rate of just under 85 percent.
Doctors with their own medical practice are most likely to still use analogue methods for the management of patient data, with 70 percent stating to have an electronic system for documentation. The marginal decline recorded for doctors with their own medical practice lies within the range of sampling error (±4.3 percent at 50/50 and probability of 95 percent).

Software use at health care facilities:
Software and electronic data processing tools are becoming ever more important as part of everyday medical and nursing activities. Among others, systems are being deployed that allow for the electronic recording of data within the user’s own organisation as well as the receipt of such data from outside this organisation. Generally speaking, considerably more data is recorded internally by all of the groups of health care professionals than can be received by institutions outside their own organisation. Viewed across all groups, demographic patient data is recorded and received most frequently. This is then followed by rather group-specific data.
Since the initial measurements were taken, the proportion of recorded and received data has increased among all health care professionals. The exception to the rule as regards the described increase are the pharmacists. Here, the figures have been stagnating for a few years (at a very high level in some cases) as they still have to communicate with other health care professionals via phone or fax.
Exchange of electronic data
In some sub-areas, exchanges between patients and health care professionals are increasingly taking place electronically, for example via encrypted e-mail. Over recent years, awareness of this necessity has obviously been on the increase among health care professionals. This is evident in the increased figures recorded among all groups since the first measurement date. Nevertheless, this communication channel has yet to establish itself as the predominant means of communication. Compared to last year, the shares recorded for most health care professionals fell slightly.
At just under 40 percent, doctors with their own medical practice are the most likely to offer such e-mail communication. They are followed by Spitex (31 percent), hospitals and hospital doctors (both 22 percent) who communicate with their patients via this channel. This communication channel is used the least by non-profit Spitex grassroots organisations and nurses with shares of just under 20 percent.

The transfer of data between patients and health care professionals should be secure.
The majority of health care professionals endeavour to comply with data protection regulations and ensure secure electronic exchanges.
Depending on the individual details provided by the groups, between around 30 percent and almost 60 percent of such communication is always conducted on a secure basis, with a further 20 percent to 35 percent usually being secured. The greatest share of secured data exchanges is reported by the hospitals (58 percent always secured and 29 percent usually secured).

In the case of all groups of health care professionals, there is still not a large offering for patients enabling them to access or view information that is saved in electronic systems themselves. The values have hardly changed since 2015.
Where the option is available, patients are, however, happy to utilise it, indicating that there is demand for such options.
Using an internationally comparable set of questions from the OECD, the status as regards internal and external networking within the surveyed groups of health care professionals was investigated. Here, it was possible to state which data has been recorded and exchanged within the individual’s own organisation (internal networking) and which data can be received from and exchanged with players from outside the organisation (external networking). Both types of networking have increased in recent years. As regards the internal networking index, it is not currently possible to identify a greater level of networking when viewed across all the respondents together. The increasing trend with respect to the external networking index has only continued minimally (advancing from 19 to 20).
Generally speaking, it is still only possible to exchange around a fifth of the conceivable data with other health care players. When the two networking types are compared, it becomes apparent at first glance that internal networking, in particular, is at an advanced stage with most health care professionals, while external networking is at a lower level. Hospitals are at the top of the list in both indices. Here, their pioneering role in the digital networking of Swiss health care becomes clear once more. As the processes of pharmacists tend to be aimed at medication data and less at other data types, their values are significantly lower than those of the other groups of health care professionals.
Attitudes toward the EPR:
General support for the EPR is this year observed among the majority of all health care professionals.
Looking at hospitals as well as old people’s homes and nursing homes, at which the EPR will be introduced in just a few years, it becomes apparent that they predominantly support the EPR. While the share of support at hospitals has even risen by almost 15 percentage points to just short of 85 percent, the value for old people’s homes and nursing homes has also increased by a few percentage points.
More than 80 percent of pharmacists support the EPR. High support values were also recorded for other groups of health care professionals, in particular among those working in a hospital environment, namely hospital doctors with just under 80 percent and nursing managers at hospitals with around 75 percent. A positive change in support for the EPR was also observed for doctors with their own medical practice, with 55 percent tending to or definitely supporting the EPR. Only among non-profit Spitex grassroots organisations was a decline in support relative to last year recorded, as support levels fell from just less than 80 percent to slightly under 70 percent.

In response to the question of what they think about the EPR to date, it becomes apparent that the majority of all health care professionals consider the EPR to be quite a good thing to a very good thing. The EPR fares best among nursing professionals, who were surveyed for the first time this year. Almost 80 percent view the EPR as quite a good thing to a very good thing. Other health care professionals, including non-profit Spitex grassroots organisations (quite/very good thing 73%), pharmacists (72%), old people’s homes and nursing homes (70%), hospitals (67%) and hospital doctors (62%), found themselves in the middle of the field with their assessments.
Doctors with their own medical practice have a critical stance with respect to the EPR and at 55% were the least likely to label the EPR a good thing. In comparison to other health care professionals, hospitals are at the most advanced stage with respect to the opinion-forming process; only a few answered with “don’t know” or failed to give an answer. Old people’s homes and nursing homes and other health care professionals are, however, not yet so advanced in their judgement, with this being especially true for hospital doctors, of whom around a quarter were still unable to provide a clear view on the EPR.

Generally speaking, the arguments in favour of the EPR were highly weighted by all health care professionals. The arguments with respect to the availability of important information in an emergency, in particular, enjoyed the most approval from health care professionals providing direct treatment (members of the medical profession, pharmacies, old people’s homes and nursing homes, non-profit Spitex organisations, nurses). Among the hospitals, primary importance is attached to the avoidance of treatment errors here, while for the cantons it is the ability to avoid unnecessary treatment and consultations.
The cantons are the only group to record the independent creation of information by patients as one of the top three arguments. The opportunity to increase the involvement of patients in the handling of their own health data is met with approval among almost all respondent groups, although this level of agreement is slightly less marked than is the case with the top three statements.
A greater level of concern is observed among members of the medical profession. Only a minority are in agreement with the statement that patients would know all of their important treatment information thanks to the EPR. In contrast to members of the medical profession working at hospitals, doctors with their own medical practices are against patients being able to create information themselves and do not expect that the quality of medical treatment would increase.
All health care professionals with the exception of members of the medical profession are in agreement with all arguments in favour of the EPR and reject all critical arguments against the EPR.
A majority of almost all health care professionals tend to trust or fully trust the bodies that work with the data relating to the EPR. The only exception here are doctors with their own practice. With a value of just shy of 45 percent, they are by far the most sceptical group of health care professionals.
Pharmacists (74 percent) and nursing professionals (73 percent) have the greatest trust in these bodies. Spitex organisations (70 percent), old people’s homes and nursing homes (69 percent) as well as hospital doctors (65 percent) revealed slightly lower levels of trust.

Health literacy:
The digitisation of the health care sector requires expertise on the part of health care professionals and patients in handling this change.
The opinion of all groups of health care professionals with respect to the qualification of their patients, home residents or clients to handle and access data is negative.
All health care professionals are predominantly of the view that the individuals to be treated are quite poorly or very poorly qualified to decide on the accessing of their data by health care professionals. This applies especially greatly to old people’s homes and nursing homes.

First interpretation:
Digitisation of health care sector stalls
Health care professionals are increasingly viewing the Internet as an opportunity for citizens with respect to usage in connection with health information. However, the processing of digitisation in the Swiss health care sector is stalling. This becomes especially clear when we look at networking between health care professionals: the internal and external networking indices have hardly changed this year and external networking, in particular, still remains at a low level. Although data is increasingly being processed electronically in some cases, the exchanging of this data with other health care professionals is not becoming any easier. For patients, there are thus hardly any opportunities to benefit additionally from this networking. The existing demand among patients for access to and the exchange of electronic health data is not being catered to. There is a gap here that could potentially be filled by the EPR.
EPR since 2017: status at hospitals and nursing homes
The Federal Act on the Electronic Patient Record entered into force in April 2017. Hospitals and nursing homes have since been required to offer their patients an EPR within a deadline of three and five years, respectively. This has left its mark on hospitals, in particular, who are strong proponents of the EPR and have also developed further in many digital areas. Developments at old people’s homes and nursing homes are still far less visible.
EPR: positive attitudes – platforms live from attractive offers and many users
Health care professionals are for the first time once again predominantly supportive of the EPR across all groups. With respect to the arguments relating to the EPR, the majority of all health care professionals come down on the positive side. All of the arguments with the most support speak in favour of the EPR, above all the availability of important information in emergency situations and the avoidance of unnecessary consultations and treatment. Concerns regarding data protection have declined relative to just last year among almost all groups. Also, with a view to the positive attitudes towards the EPR among the population, the EPR thus has the potential to serve as an important interface between health care professionals and patients and to meet the demand for interaction possibilities. To this end, however, a large number of users are required at all age levels.
Members of the medical profession
Members of the medical profession have their concerns with respect to the digitisation of health care but are gradually opening up to the efforts being made in the area of eHealth. In some respects, they are the most advanced group to date as regards exchanges between health care professionals and patients, for example offering patients encrypted e-mail communication or allowing them to perform activities online. In other digitisation segments, as well as for the EPR, there is still potential for members of the medical profession, especially with respect to the benefits of the EPR. A clear indication that members of the medical profession need to be involved in the designing of the EPR.
Hospitals
Hospitals are still playing a pioneering role in the digitisation of the Swiss health care sector. The Federal Act on the Electronic Patient Record in the past initiated various processes that helped to propel hospitals into a leading position among health care professionals in the area of eHealth, for example the electronic performance of functions and networking within and outside respondents’ own organisations. Next steps would now include transferring this to other hospital-based health care professionals.
Pharmacists
Pharmacists are leaders in some areas of digitisation, for example the use of the electronic vaccination record. However, they are only progressing slowly in other respects. While the need for pharmacists to exchange medication data with other health care professionals and patients remains great, communication with other specialists relating to medication unfortunately still very often takes place via phone or fax. As was the case previously, pharmacists are the health care professionals most likely to recommend the EPR. This prevailing mood can be utilised to initiate further steps in the implementation of the EPR as well as digitisation among pharmacists.
Old people’s homes and nursing homes
Since the introduction of the Federal Act on the Electronic Patient Record, there has as yet been little change in the situation at nursing homes, a fact that can probably also be explained by the slightly longer deadline for its introduction than at hospitals. Generally speaking, there is a positive attitude towards the EPR. The level of internal and external networking has fallen slightly compared to last year. A clear increase was recorded with respect to eHealth strategies.
Non-profit Spitex organisations
Electronic documentation is being introduced to a growing extent by the Spitex grassroots organisations, which have recorded the biggest increase relative to the other health care professionals. While internal networking has reduced slightly, external networking has increased. This underlines the desire for more exchanges with other health care professionals. Nevertheless, support for the EPR has decreased slightly, a development that is possibly linked to the difficulties experienced in exchanging data with other specialists. However, of all the health care professionals, non-profit Spitex organisations registered the highest increase in memberships to (core) associations this year. This means there is a positive outlook for the future.
Nursing
The hospitals’ nursing services benefit in part from the hospital-related environment in which they operate. This is especially true with respect to the existence of eHealth strategies, electronic documentation and internal and external networking. There is also a desire for greater data exchanges with other health care professionals here. Both the degree of support for the EPR and the level of trust that the data in the EPR is protected are very high. Nursing services are at an advanced stage when it comes to the networked handling of electronic data in exchanges with other health care professionals. This means there is a positive outlook for the future with respect to the implementation of the EPR.
Cantons
The targeted organisation of health care professionals within (core) associations is largely taking place at a cantonal level. Nevertheless, the cantons will need to seek a leading role in the environment of core associations if they want to see the EPR definitively pass into the productive phase.
Methodological details:
Company: InfoSocietyDays
Survey population: doctors, people responsible for IT at hospitals, pharmacists, old people’s homes and nursing homes, people responsible for eHealth at a cantonal levels, members of Spitex Switzerland, nursing professionals
Survey area: the whole of Switzerland (three languages)
Origin of the addresses: doctors: Swiss Medical Association, hospitals: InfoSocietyDays, pharmacists: pharmaSuisse, old people’s homes and nursing homes: CURAVIVA, cantons: eHealth Suisse (contact directly via eHealth Suisse), Spitex: Swiss Spitex Association, nursing professionals: Careum Foundation
Data collection: online, also print for doctors
Type of sampling procedure: at random/complete survey
Survey period: 1 December 2018 to 20 January 2019 (mean survey date: 26 December 2018)
Sample size: doctors: 785 (doctors with their own practice: 551, hospital doctors: 150, hospital doctors also with their own practice: 52), hospitals: 72, pharmacists: 342, old people’s homes and nursing homes: 440, cantons: 22, non-profit Spitex organisations: 122, nursing professionals: 49
Weighting: none